Learning points
- Belching can be classified into two types, gastric belching and supragastric belching (SGB). The former is the physiological reflex to vent accumulated air in the stomach, whereas the latter is an unconscious behavioural disorder.
- SGB patients can also complain about predominant reflux symptoms rather than increased belching.
- Impedance-pH monitoring can objectively distinguish the two types of belching.
- Cognitive behavioural therapy (CBT) using diaphragmatic breathing is the best-established treatment for excessive SGB. Up to 60% of patients with SGB can respond to CBT satisfactorily.
Case study
A 46-year-old male was referred to the gastroenterology department due to bothersome belching lasting for one and a half years. Occasional heartburn coincided with the belching episodes. Otherwise, he did not have any other symptoms or medical conditions. His belching constantly occurred even during the medical interview, except for when he was answering questions. His upper GI endoscopy was normal.
Discussion
There are two types of belching, gastric belching (GB) and supragastric belching (SGB). GB is a physiological reflex to vent accumulated air in the stomach via transient lower oesophageal sphincter relaxation, whilst SGB is an unconscious but voluntary behaviour involving immediate expulsion of swallowed air in the oesophagus using the abdominal straining [1]. Belching can be bothersome when excessive. Indeed, excessive SGB impairs quality of life [2]. Both types of excessive belching are classified in functional gastroduodenal disorders according to Rome IV [3].
Not only GB but also SGB are closely related to GORD. SGB can induce gastroesophageal reflux, and consequently patients with excessive SGB often predominantly suffer from reflux symptoms rather than belching symptoms [4]. Up to 40% of patients referred to a tertiary centre due to PPI-refractory reflux symptoms had excessive SGB [5]. Additionally, SGB was responsible for approximately one-third of oesophageal acid burden [6].
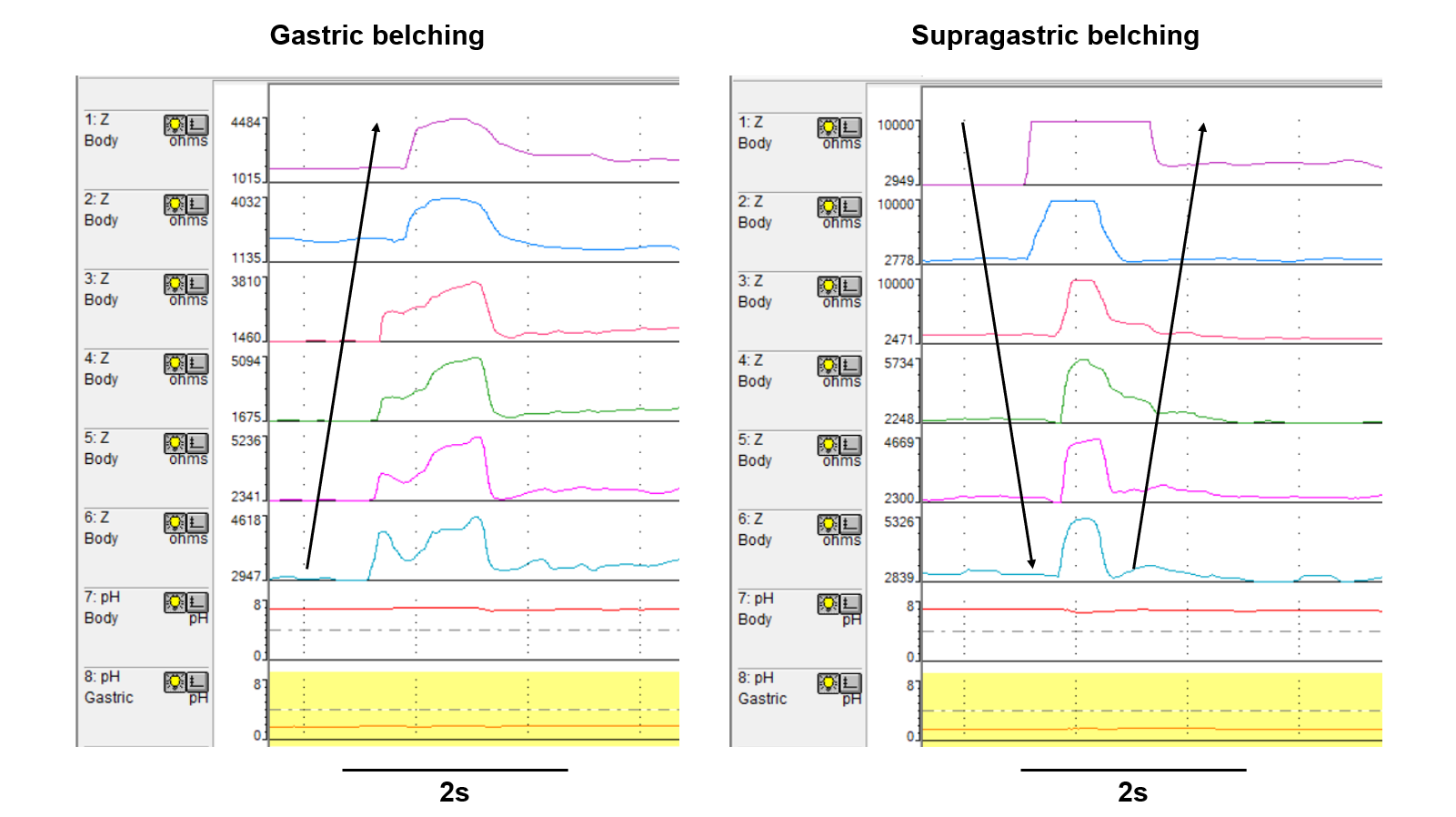
For appropriate management, it is essential to precisely identify the type of belching. Looking at a patient’s history can provide a clue on the diagnosis as continual belching strongly suggests the possibility of SGB. However, objective testing should not be omitted because it is the only way to make a definitive diagnosis of excessive SGB. Impedance-pH monitoring can objectively distinguish the two types of belching (please see the image above in the answer to question 2). Healthy volunteer data indicates SGB>13 episodes/24h is pathological, although the necessity of the treatment depends on symptom burden [7].
CBT or speech therapy using diaphragmatic breathing is the mainstay of the treatment for excessive SGB [4, 8, 9]. CBT can alleviate severity of belching symptoms satisfactorily in up to 60% of patients, along with the reduction of SGB. CBT also reduced concomitant pathological acid exposure from 9.0±3.2% to 6.1±3.5% [4]. CBT consists of cognitive and behavioural parts [4]. The former helps the patients understand the mechanism of SGB and how CBT works on SGB, in addition to realising a warning signal prior to a burst of SGB (e.g. epigastric discomfort). The latter teaches them diaphragmatic breathing techniques with mouth opening to physically stop SGB. A randomised control trial failed to show the efficacy of baclofen on SGB [1].
Regarding the treatment for GB, lifestyle modification such as eating slowly might reduce aerophagia. Baclofen can improve GB via inhibition of transient lower oesophageal sphincter relaxation [10].
Images legend
In impedance-pH monitoring, gastric belching can be seen as rise of impedance (i.e. air) moving from the bottom (i.e. the distal oesophagus) to the top (i.e. the proximal oesophagus). Supragastric belching shows V-shaped impedance rise which reflects swallowed air moving aborally followed by being orally expelled from the oesophagus. Black arrows indicate the direction of air movement.
Author biographies
Dr Akinari Sawada
Dr Akinari Sawada is a Consultant Gastroenterologist at Osaka Metropolitan University Hospital in Japan. He graduated from Osaka City University in 2009 and obtained a PhD in Medicine in 2017. He was an honorary GI physiologist at Royal London Hospital from 2018 to 2020 and a Clinical Lecturer at Barts and the London School of Medicine & Dentistry, Queen Mary, University of London from 2019 to 2020. His research focuses on benign oesophageal disorders and GI physiology with a special interest in gastro-oesophageal reflux disease, eosinophilic oesophagitis and achalasia.
Prof Daniel Sifrim

Prof Daniel Sifrim is a Gastroenterologist, trained in Argentina and Belgium, with both clinical and scientific interest in oesophageal benign disorders. He contributed with the development of diagnostic techniques for oesophageal motility disorders and gastro-oesophageal reflux disease (high resolution manometry, oesophageal impedance and salivary pepsin measurements). He is Emeritus Professor of Gastrointestinal Physiology at Barts and the London School of Medicine, Queen Mary University. He is co-director of the Neuro-gastroenterology Department at Princess Grace Hospital, London. He has published more than 250 articles in international peer reviewed journals and is an opinion leader in pathophysiology, diagnostic techniques and management of benign oesophageal disorders.
Q&A
-
Answer is c.
SGB is characterised by a behavioural disorder where a patient swallows or sucks air from the mouth into the oesophagus, immediately followed by expulsion of the air from the oesophagus using the abdominal straining. SGB rarely occurs during speaking since the air physically cannot be swallowed.
-
Answer is b.
pH-Impedance monitoring can evaluate the movement of air and liquid in the oesophagus. Using MII-pH, the two types of belching can be objectively distinguished (please see the image below). Patients with SGB usually have a series of frequent repetitive belching, however the clinical distinction between gastric and supragastric belching is difficult. HRM, wireless pH monitoring, or gastric emptying tests cannot diagnose SGB properly.
-
Answer is a.
CBT is the mainstream therapy for SGB due to non-invasiveness and high efficacy. Baclofen, g-aminobutyric acid analogue, was not very effective for SGB in a previous randomised controlled trial. For this patient, absence of erosive esophagitis or reflux symptoms does not justify the use of PPIs or fundoplication. Conversely, fundoplication is known to increase SGBs postoperatively.
CME
Clinical updates on the diagnosis and management of functional dyspepsia
02 January 2024
Cyclic Vomiting Syndrome
03 October 2023
ARFIDs and DGBI: Trying to make practical sense from the collision of two heterogeneous conditions
01 August 2023
[1] Sawada A, Fujiwara Y, Sifrim D. Belching in Gastroesophageal Reflux Disease: Literature Review. J Clin Med 2020; 9.
[2] Bredenoord AJ, Smout AJ. Impaired health-related quality of life in patients with excessive supragastric belching. Eur J Gastroenterol Hepatol 2010; 22:1420-1423.
[3] Stanghellini V, Chan FK, Hasler WL et al. Gastroduodenal Disorders. Gastroenterology 2016; 150:1380-1392.
[4] Glasinovic E, Wynter E, Arguero J et al. Treatment of supragastric belching with cognitive behavioral therapy improves quality of life and reduces acid gastroesophageal reflux. Am J Gastroenterol 2018; 113:539-547.
[5] Sawada A, Guzman M, Nikaki K et al. Identification of Different Phenotypes of Esophageal Reflux Hypersensitivity and Implications for Treatment. Clin Gastroenterol Hepatol 2020.
[6] Sergeev I, Velosa M, Mardare R et al. The influence of supragastric belching severity on esophageal acid exposure and motility. Neurogastroenterol Motil 2022:e14520.
[7] Koukias N, Woodland P, Yazaki E, Sifrim D. Supragastric Belching: Prevalence and Association With Gastroesophageal Reflux Disease and Esophageal Hypomotility. J Neurogastroenterol Motil 2015; 21:398-403.
[8] Hemmink GJ, Ten Cate L, Bredenoord AJ et al. Speech therapy in patients with excessive supragastric belching–a pilot study. Neurogastroenterol Motil 2010; 22:24-28, e22-23.
[9] Ong AM, Chua LT, Khor CJ et al. Diaphragmatic Breathing Reduces Belching and Proton Pump Inhibitor Refractory Gastroesophageal Reflux Symptoms. Clin Gastroenterol Hepatol 2018; 16:407-416.e402.
[10] Cossentino MJ, Mann K, Armbruster SP et al. Randomised clinical trial: the effect of baclofen in patients with gastro-oesophageal reflux–a randomised prospective study. Aliment Pharmacol Ther 2012; 35:1036-1044.
